If you’ve been diagnosed with fibromyalgia, you know better than anyone the pain, frustration and anxiety associated with this difficult to define disease. Ask anyone what the worst part about fibromyalgia (FMS) is and they might list the numbness, pain, difficulty sleeping, irritable bowel syndrome and the persistent depression – or they might say the worst part is simply not knowing the cause.
Some experts believe FMS is related to “illness,” trauma or just plain stress. Others link the condition to hormonal disturbances and chemical imbalances affecting the nervous system. Still other researchers blame genetic ties or claim there is no explanation at all. But what if there was an option D, “all of the above?” Clinical experience and in-depth testing have begun to point to Lyme disease complex, coinfections and weakened immunity, which could answer that question.
What is Lyme Disease?
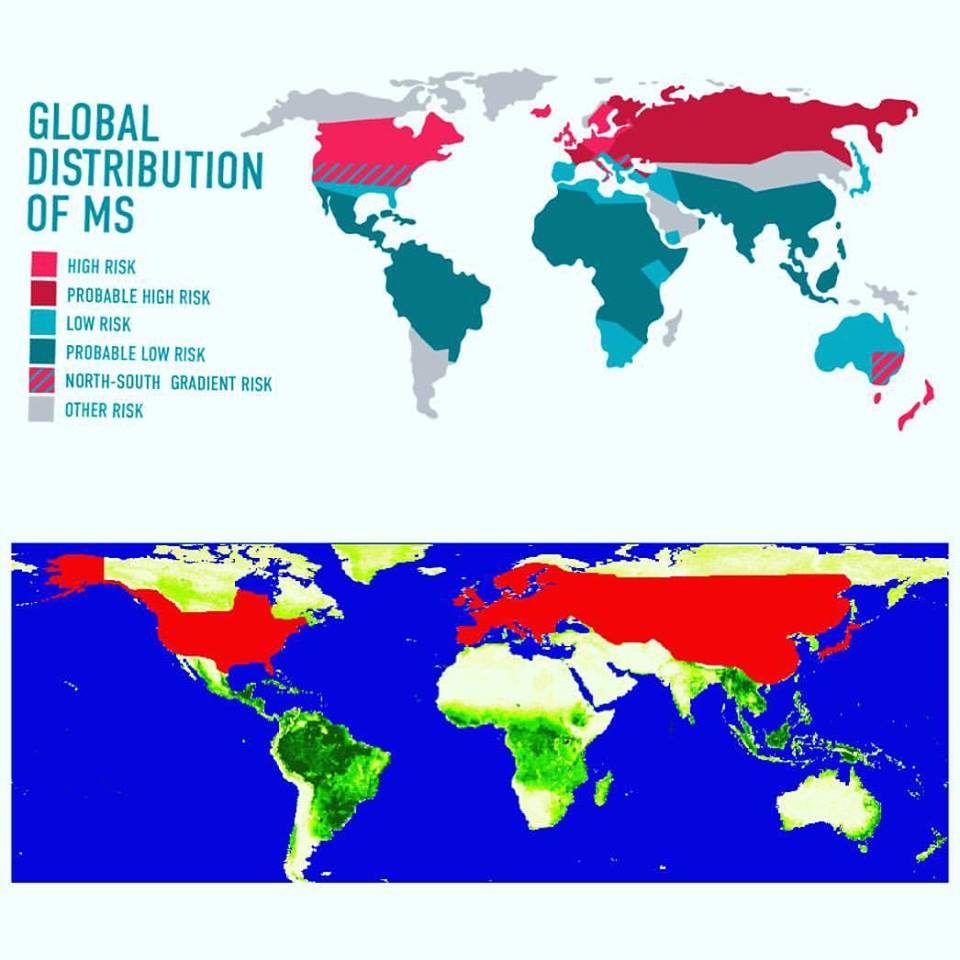
Lyme disease is most famously transferred through insect bites, particularly ticks. As a cousin to syphilis, it may spread from a mother to her fetus or through sexual contact, but this connection has not yet been proven.
Lyme is characterized by a spirochete infection called Borrelia, which is a tube-like bacterium that works by releasing bacterial lipoproteins (BLPs). These BLPs are a type of neurotoxin that lead to memory problems; hormonal imbalances; burning neurological pain; generalized inflammation; gastrointestinal discomfort and numbness; not to mention symptoms like swollen lymph nodes; fever and chills; headache and stiff neck; muscle and joint paint; and the most common symptom, lack of energy.
A spirochete is covered in antigens, which act like fingerprints, identifying itself to the immune system. When your Killer T Cells find these antigens, they know to destroy the invading bacteria. However, when the borrelia spirochete burrows into the body, its antigens are smeared over healthy tissue, which the killer T cells attack because they cannot differentiate between healthy and unhealthy tissue. When this happens, it’s called an “autoimmune disease.” This is one explanation that may describe why borrelia and its coinfections can be commonly found in autoimmune and rheumatic disease patients.
The more the spirochete moves through the body, the more BLPs it releases, impairing the immune system, creating inflammations, irritations and wreaking havoc to the peripheral and central nervous systems and the entire neural endocrine system. As a result, Lyme disease and its coinfections can be associated with more than 300 other diseases, including chronic fatigue syndrome and numerous autoimmune diseases.
Linking Fibromyalgia and Lyme Disease Complex
As you can see, early stages of Lyme disease complex can be very difficult to diagnose, even with a blood test. In addition to physical examination results, most doctors will rely on environmental factors such as exposure to ticks and medical history (according to Medscape, only 25-30% of patients recall a tick bite.) But let’s go back to fibromyalgia. Some of these symptoms certainly overlap, especially muscle pain and fatigue, but is there a link?
According to one author on Fibromyalgia.com, “…long-term joint problems can be activated and this can lead to a central sensitization syndrome (the central pain amplifier being turned up) … I still can’t give you a positive “yes” or “no” but I suspect there is a potential for a link.”
Also, consider the connection between Chronic Fatigue Syndrome (CFS) and FMS through the Hypothalamic-pituitary-adrenal axis. Don’t let that long string of words confuse you – the HPA is merely a communication network of direct influences and feedback interactions between the hypothalamus, the pituitary gland and the adrenal gland. Think of it as an Internet connection in your brain that controls the master hormones of the body. In many cases, abnormal levels of certain chemicals that are regulated by the HPA axis have been proposed as a potential cause of CFS.
The way this relates to Lyme disease complex is quite interesting. Patients can contract an infection at any point in their lifetime, but the symptoms can very well lay dormant until the individual is weakened (immune compromised), usually by a traumatic experience such as a major injury, giving birth, receiving a vaccine or even extreme emotional trauma such as divorce or death. Such trauma will undoubtedly affect the HPA axis, however, how much will vary depending on the patient.
The HPA axis is where experts have argued there is a genetic link to FMS. However, with infections, it may be less genetic and more epigenetic, which means an outside influence changes gene expression, which is typically seen in cancerous cells.
Let’s bring it all back – Chronic Lyme disease complex can affect the Hypothalamic-pituitary-adrenal axis in two ways: via neurotoxins and epigenetic shifts. So if imbalances in the HPA axis can lead to Chronic Fatigue Syndrome, depression, insomnia and generalized pain, all of which is related to fibromyalgia, then it seems there is a strong link from Lyme disease complex and its coinfections to FMS.
Finding the Proper Treatment
You may find that treating Lyme disease complex is not easy at all. If it’s caught early, antibiotics may nip the problem in the bud. However, this is rarely the case, if Lyme disease is detected at all. Second, the oral antibiotics are usually administrated in a 4-to-6 week period, meaning once that treatment ends, the borrelia will make a comeback, causing the patient to relapse. Furthermore, the antibiotics do not strengthen the immune system and do little to address the coinfections, the secondary infections, the BLP neurotoxins or strip away the protective biofilm, which is a sludge produced by the bacteria to protect itself from antibiotics.
Sometimes patients will include supplements with their antibiotics. In this scenario, the infection will be brought down a little and the supplements will slightly increase the immune system. But again, if the immune system is completely established and all the infections are brought down to lower levels, relapse will occur.
The Lyme disease complex involves a multitude of infections that may also include other complications such as chemical and heavy metal toxicities. If you really want to nuke Lyme disease and its coinfections, it’s ideal to have a combination of advanced immunotherapy, aggressive natural antiviral, antifungal, IV antibiotics and biodetoxification. When this is provided by the properly trained integrative physician in a customized treatment plan, these therapies will help bring the patient back to optimal health.
The final step is utilizing the biodetoxification process in order to rid the body of the neurotoxins and the BLPs. Ultimately the neurotoxins are competing with every nerve and hormone receptor within the patient’s body. Follow-up care may involve hormone balancing, neurotransmitter and immune system support.